August 2024
It's Time for Beautiful Feet
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Possible Causes and Treatments of Plantar Fasciitis

The plantar fascia is a long, thick band of tissue that spans from the heel bone along the bottom of the foot to the toes. The plantar fascia supports the bottom of the feet and toes during walking, running, and jumping. It can become overly stressed, or even tear or rupture, from overuse or injury that causes pain and inflammation, termed plantar fasciitis. Being obese, standing or working on your feet for prolonged periods of time, or having flat feet or high arches can all contribute to this condition. Engaging in activities that involve dancing, marching, or running can also add to, or possibly worsen, the symptoms of plantar fasciitis. Certain footwear, such as high heels, flip flops, worn out shoes, or other types of footwear with inadequate support, can also increase the risk of developing this condition. A podiatrist will use a variety of ways to treat plantar fasciitis depending upon the severity of the condition and how long the patient has been suffering from it. If you have been dealing with pain from plantar fasciitis, it is suggested you schedule an appointment with a podiatrist for a diagnosis and comprehensive treatment plan.
Plantar fasciitis is a common foot condition that is often caused by a strain injury. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Robert Marcus from Foot & Ankle Center of Teaneck. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is one of the most common causes of heel pain. The plantar fascia is a ligament that connects your heel to the front of your foot. When this ligament becomes inflamed, plantar fasciitis is the result. If you have plantar fasciitis you will have a stabbing pain that usually occurs with your first steps in the morning. As the day progresses and you walk around more, this pain will start to disappear, but it will return after long periods of standing or sitting.
What Causes Plantar Fasciitis?
- Excessive running
- Having high arches in your feet
- Other foot issues such as flat feet
- Pregnancy (due to the sudden weight gain)
- Being on your feet very often
There are some risk factors that may make you more likely to develop plantar fasciitis compared to others. The condition most commonly affects adults between the ages of 40 and 60. It also tends to affect people who are obese because the extra pounds result in extra stress being placed on the plantar fascia.
Prevention
- Take good care of your feet – Wear shoes that have good arch support and heel cushioning.
- Maintain a healthy weight
- If you are a runner, alternate running with other sports that won’t cause heel pain
There are a variety of treatment options available for plantar fasciitis along with the pain that accompanies it. Additionally, physical therapy is a very important component in the treatment process. It is important that you meet with your podiatrist to determine which treatment option is best for you.
If you have any questions, please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
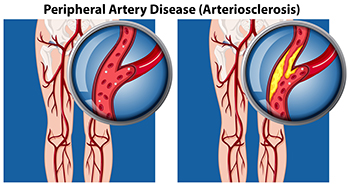
Peripheral Artery Disease
Peripheral artery disease (PAD), or peripheral arterial disease, is a circulatory problem in which there is a reduction of blood flow to the limbs due to narrowed arteries. When peripheral artery disease develops, the extremities do not receive enough blood flow; this may cause symptoms to develop such as claudication, or leg pain when walking. The legs are the most common site of peripheral artery disease.
Claudication, or leg pain when walking, is one of several symptoms that can develop due to peripheral artery disease. Other symptoms caused by the disease include painful cramping in the hips, thighs, or calves after certain activities; leg numbness or weakness; coldness in the lower leg or foot; sores on the lower extremities that do not heal; hair loss on the lower extremities; and a missing or weak pulse in the lower extremities. In more severe cases, pain may even occur when the body is at rest or when lying down.
Peripheral artery disease is typically caused by atherosclerosis, a condition in which fatty deposits build up in the arterial walls and reduce blood flow. Smoking, diabetes, obesity, high blood pressure, and high cholesterol are some of the risk factors for peripheral artery disease.
If you are experiencing pain, numbness, or other symptoms in the lower extremities, see your healthcare professional immediately. Diagnosed peripheral artery disease can be treated with various medications, angioplasty and surgery, exercise programs, or alternative medicine. It is important to consult a healthcare professional to determine the best treatment for you.
Peripheral Artery Disease and the Feet
Peripheral artery disease, or PAD, can significantly affect the feet, often causing pain, even during normal activities like walking. This discomfort, medically known as claudication, occurs because of reduced blood flow due to plaque buildup in the arteries. Symptoms of PAD in the feet include cramps, numbness, skin discoloration, temperature changes, and the development of ulcers. These symptoms are concerning because they indicate insufficient blood circulation, which, if untreated, could lead to serious conditions like limb ischemia. In severe cases, this can result in tissue death or even amputation. It is vital for individuals with peripheral artery disease to engage in regular, supervised exercise to improve circulation. A podiatrist can help to manage the effects of PAD by providing specialized foot care, monitoring symptoms, and advising on exercise programs tailored to enhance blood flow. They can also guide patients in footwear choices and care for ulcers to prevent infections. If you have foot problems related to peripheral artery disease, it is suggested that you schedule an appointment with a podiatrist for treatment.
Peripheral artery disease can pose a serious risk to your health. It can increase the risk of stroke and heart attack. If you have symptoms of peripheral artery disease, consult with Dr. Robert Marcus from Foot & Ankle Center of Teaneck. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
Peripheral artery disease (PAD) is when arteries are constricted due to plaque (fatty deposits) build-up. This results in less blood flow to the legs and other extremities. The main cause of PAD is atherosclerosis, in which plaque builds up in the arteries.
Symptoms
Symptoms of PAD include:
- Claudication (leg pain from walking)
- Numbness in legs
- Decrease in growth of leg hair and toenails
- Paleness of the skin
- Erectile dysfunction
- Sores and wounds on legs and feet that won’t heal
- Coldness in one leg
It is important to note that a majority of individuals never show any symptoms of PAD.
Diagnosis
While PAD occurs in the legs and arteries, Podiatrists can diagnose PAD. Podiatrists utilize a test called an ankle-brachial index (ABI). An ABI test compares blood pressure in your arm to you ankle to see if any abnormality occurs. Ultrasound and imaging devices may also be used.
Treatment
Fortunately, lifestyle changes such as maintaining a healthy diet, exercising, managing cholesterol and blood sugar levels, and quitting smoking, can all treat PAD. Medications that prevent clots from occurring can be prescribed. Finally, in some cases, surgery may be recommended.
If you have any questions, please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
How to Handle a Long Work Day on Your Feet
In 2014, the American Podiatric Medical Association surveyed 1,000 American adults and found that half of all respondents lived with foot pain. Fortunately, there are ways to avoid foot problems such as following a daily footcare routine and wearing proper footwear at work.
If you have a job that requires you to be on your feet, it is best that you do not wear flat sole shoes. Your heel should be slightly elevated (less than 2 inches, but at least ¼-inch) if you are going to be standing for a prolonged period. You should also make sure that the shoes you wear are not too small. Tight shoes may cut off circulation to your feet, which will result in pain and blisters. It is always best to purchase fitted shoes later in the day, because the feet tend to swell as the day progresses. It may also be helpful to buy shoes a half size larger if you plan on wearing custom orthotics or arch supports.
Your muscles may become stiff when you are constantly standing up. It is important to take breaks every hour to stretch and relax. One tip is to perform calf raises, because this exercise will help improve your circulation. To perform this stretch, you first need to stand on the edge of a step with your abdominal muscles pulled inward. You then need to grip the step with the balls of your feet with your heels hanging over the edge. Next, try to raise your heels above the step by a few inches while standing on your tiptoes; hold this pose for a second. You should then lower your heels back even to the platform. These calf raises should be done ten times for full effectiveness.
You should also take care of your feet while you are at home. One of the best ways to prepare your feet for a long day of work is to soak them in ice water. Doing so for 20 minutes will help fight the swelling and inflammation that results from being on your feet at work.
Nevertheless, if you are experiencing pain in your feet, you should seek help from your podiatrist. Your doctor will help treat any ailments you may have in addition to helping you prevent any other ailments from developing in the future.
Proper Footwear for Restaurant Workers

Proper footwear is essential for restaurant workers as a way of maintaining health and comfort throughout long shifts. These jobs often involve extended periods of standing and walking on hard surfaces, which can lead to foot, leg, and back pain if the right shoes are not worn. Proper footwear provides necessary support, cushioning, and stability, helping to absorb shock and reduce the risk of injuries such as sprains or stress fractures. Shoes with slip-resistant soles also enhance safety by preventing slips and falls in potentially hazardous kitchen environments. Additionally, wearing well-fitted, supportive shoes can help alleviate common issues like plantar fasciitis and bunions. Investing in high-quality, ergonomic footwear ensures that restaurant workers remain comfortable and protected. If you work in the restaurant industry and have endured a foot injury or have developed chronic foot pain, it is suggested that you speak with a podiatrist. This type of doctor can offer effective treatment options, in addition to guiding you toward wearing appropriate footwear for the job.
While working on the feet, it is important to take the proper care of them. For more information about working on your feet, contact Dr. Robert Marcus from Foot & Ankle Center of Teaneck. Our doctor will treat your foot and ankle needs.
Working on Your Feet
Standing on your feet for long periods of time can cause stress and pain in your feet. Your whole body may experience change in terms of posture, back pain, bunions, callouses and or plantar warts. There are ways to avoid these conditions with proper foot care, smart choices and correct posture.
Positive Changes
Negative heeled shoe – Choosing this shoe type places the heel slightly lower than the ball of the foot. These are great for overall foot health. Find shoes that fit you correctly.
Go barefoot – Our feet were not designed to be enclosed for all hours of the day. Try to periodically expose your feet to air.
Eliminate Pain
Foot Exercises – Performing simple exercises, incorporating yoga and doing stretches are beneficial. This will allow increased blood flow to the area and muscles of the foot.
Achilles tendon – Stretching the foot out flat on the floor will relax the calf muscles and tendon. These exercises can be performed almost anywhere. Make sure you add these exercises to your daily regimen.
With a little bit of this information and knowing more about foot health, you will notice changes. Foot stretches and proper footwear will help with pain and prevent further issues.
If you have any questions please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Wound Care
Diabetics must be wary of all wounds, regardless of depth or size. Diabetes, a chronic disease in which the body cannot properly use glucose the way it normally would, causes various complications that make wounds difficult to heal. Nerve damage or neuropathy will cause diabetics to have trouble feeling the pain of a blister or cut until the condition has significantly worsened or become infected. A diabetic’s weakened immune system can make even the most minor of wounds easily susceptible to infection. Diabetics are also more prone to developing narrow, clogged arteries, and are therefore more likely to develop wounds.
Wounds should be taken care of immediately after discovery, as even the smallest of wounds can become infected if enough bacteria build up within the wound. To remove dirt, wounds should be first rinsed under running water only. Soap, hydrogen peroxide, or iodine can irritate the injury and should be avoided. To prevent infection, apply antibiotic ointment to the wound and cover it with a bandage. The bandage should be changed daily. The skin around the wound may be cleaned with soap.
To prevent further exacerbation, see a doctor—especially if you have diabetes. Minor skin conditions can become larger problems if not properly inspected. As the wound heals, make sure to avoid applying pressure to the affected area.
Recognition and Treatment of Infected Foot Wounds
 Recognizing an infected foot wound is essential for prompt treatment and prevention of serious complications. Signs of infection include increased redness, swelling, warmth around the wound, and persistent pain. The wound may also produce pus or an unpleasant odor, and systemic symptoms such as fever or chills can occur. Immediate treatment involves thoroughly cleaning the wound with mild soap and water. Applying an antiseptic solution helps reduce bacterial load. Cover the wound with a sterile bandage and change it daily or as needed to keep it clean and dry. Mild pain relievers can help manage discomfort. Individuals with diabetes or compromised immune systems should be particularly vigilant, as they are at higher risk for complications. Early intervention and proper care are key to effectively treating an infected foot wound and promoting healing. If you have a foot wound and it appears infected or does not heal properly, it is strongly suggested that you schedule an appointment with a podiatrist as soon as possible for antibiotics or advanced wound care techniques.
Recognizing an infected foot wound is essential for prompt treatment and prevention of serious complications. Signs of infection include increased redness, swelling, warmth around the wound, and persistent pain. The wound may also produce pus or an unpleasant odor, and systemic symptoms such as fever or chills can occur. Immediate treatment involves thoroughly cleaning the wound with mild soap and water. Applying an antiseptic solution helps reduce bacterial load. Cover the wound with a sterile bandage and change it daily or as needed to keep it clean and dry. Mild pain relievers can help manage discomfort. Individuals with diabetes or compromised immune systems should be particularly vigilant, as they are at higher risk for complications. Early intervention and proper care are key to effectively treating an infected foot wound and promoting healing. If you have a foot wound and it appears infected or does not heal properly, it is strongly suggested that you schedule an appointment with a podiatrist as soon as possible for antibiotics or advanced wound care techniques.
Wound care is an important part in dealing with diabetes. If you have diabetes and a foot wound or would like more information about wound care for diabetics, consult with Dr. Robert Marcus from Foot & Ankle Center of Teaneck. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
What Is Wound Care?
Wound care is the practice of taking proper care of a wound. This can range from the smallest to the largest of wounds. While everyone can benefit from proper wound care, it is much more important for diabetics. Diabetics often suffer from poor blood circulation which causes wounds to heal much slower than they would in a non-diabetic.
What Is the Importance of Wound Care?
While it may not seem apparent with small ulcers on the foot, for diabetics, any size ulcer can become infected. Diabetics often also suffer from neuropathy, or nerve loss. This means they might not even feel when they have an ulcer on their foot. If the wound becomes severely infected, amputation may be necessary. Therefore, it is of the upmost importance to properly care for any and all foot wounds.
How to Care for Wounds
The best way to care for foot wounds is to prevent them. For diabetics, this means daily inspections of the feet for any signs of abnormalities or ulcers. It is also recommended to see a podiatrist several times a year for a foot inspection. If you do have an ulcer, run the wound under water to clear dirt from the wound; then apply antibiotic ointment to the wound and cover with a bandage. Bandages should be changed daily and keeping pressure off the wound is smart. It is advised to see a podiatrist, who can keep an eye on it.
If you have any questions, please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.