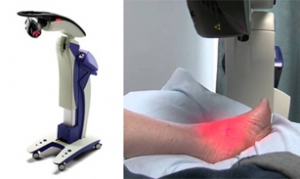
A Laser Treatment for Pain Relief
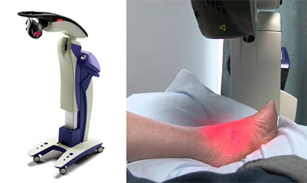 Multiwave Locked System known as MLS laser therapy, is a safe, noninvasive and effective treatment for various chronic and acute injuries. MLS uses different wavelengths of light to relieve pain and reduce inflammation in the affected areas. Light energy from the laser penetrates the tissue and enters damaged cells to stimulate cell activity and promote healing. It can be used for many conditions of the foot and ankle, such as tendon and ligament injuries, muscle strains and tears, ligament sprains, sore muscles and joints, neurological pain, and diabetic pain. MLS laser therapy can provide rapid pain relief without negative side effects and soft tissue repair can be stronger and faster. For more information about MLS laser therapy, consult with a podiatrist today.
Multiwave Locked System known as MLS laser therapy, is a safe, noninvasive and effective treatment for various chronic and acute injuries. MLS uses different wavelengths of light to relieve pain and reduce inflammation in the affected areas. Light energy from the laser penetrates the tissue and enters damaged cells to stimulate cell activity and promote healing. It can be used for many conditions of the foot and ankle, such as tendon and ligament injuries, muscle strains and tears, ligament sprains, sore muscles and joints, neurological pain, and diabetic pain. MLS laser therapy can provide rapid pain relief without negative side effects and soft tissue repair can be stronger and faster. For more information about MLS laser therapy, consult with a podiatrist today.
MLS Laser Therapy is a successful alternative for treating any pain you may be experiencing related to certain podiatric conditions. If you are interested in MLS Laser Therapy, consult with Dr. Robert Marcus from Foot & Ankle Center of Teaneck. Our doctor will assess your condition and provide you with quality foot and ankle treatment.
MLS Laser Therapy
Multiwave Locked System (MLS) Laser Therapy is a patented, FDA-cleared technology that helps relieve pain and inflammation from a number of podiatric conditions, including:
- Heel Pain
- Plantar Fasciitis
- Sports Injuries
- Wounds
- Achilles Tendonitis
- Arthritis
- Neuropathy
- Neuromas
MLS Laser Therapy is an ideal alternative to surgery and prescription medication, as it has no negative side effects and encourages accelerated healing. Among its many clinical benefits, MLS Laser Therapy also:
- Reduces swelling due to bruising or inflammation
- Blocks pain
- Reduces formation of scar tissue
- Improves nerve function
If you have any questions, please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
MLS Laser Therapy
MLS Laser Therapy is an FDA-approved technology designed to treat various painful conditions. It is often sought out as a successful alternative to surgical treatment and prescription medication that may otherwise bring about negative side effects. During MLS Laser Therapy, light energy enters the damaged cells to stimulate intercellular activity, reducing pain in the affected area and accelerating the recovery process.
MLS Laser Therapy is used in podiatry to treat various conditions. These include heel pain, plantar fasciitis, sports injuries, wounds, Achilles tendonitis, arthritis, neuromas, neurological pain, musculoskeletal disorders, and sore muscles. Aside from the specific conditions MLS Laser Therapy treats, patients can also gain from the treatment’s general benefits. These benefits include a rapid relief of pain, the reduction of swelling caused by inflammation or bruising, faster healing, improved blood circulation, the reduction of scar tissue, and improved nerve function.
MLS Laser Therapy is a non-surgical treatment with no side effects. The treatment process is painless and typically takes a short amount of time to complete. Several treatments may be required depending on the specific condition.
What Is Causing My Heel Pain?
 Heel pain when first getting out of bed in the morning, a burning or sharp sensation in the heel, and increased pain while walking, can all be indicative of the foot condition known as plantar fasciitis. Plantar fasciitis can be an uncomfortable foot condition to deal with, especially if it is left untreated. Common causes of this condition can include ill-fitting footwear, poor foot structure, certain exercises like long distance running, and occupations that require you to be on your feet for the majority of the day. Obesity may also lead to the development of plantar fasciitis, due to the excess pressure put on the foot. If you have heel pain, please seek the care of a podiatrist immediately for a proper diagnosis.
Heel pain when first getting out of bed in the morning, a burning or sharp sensation in the heel, and increased pain while walking, can all be indicative of the foot condition known as plantar fasciitis. Plantar fasciitis can be an uncomfortable foot condition to deal with, especially if it is left untreated. Common causes of this condition can include ill-fitting footwear, poor foot structure, certain exercises like long distance running, and occupations that require you to be on your feet for the majority of the day. Obesity may also lead to the development of plantar fasciitis, due to the excess pressure put on the foot. If you have heel pain, please seek the care of a podiatrist immediately for a proper diagnosis.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact Dr. Robert Marcus from Foot & Ankle Center of Teaneck. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Athlete's Foot
Athlete’s foot is an extremely contagious infection caused by a fungus that results in itching, burning, dry, and flaking feet. The fungus that causes athlete’s foot is known as tinea pedis and thrives in moist, dark areas such as shower floors, gyms, socks and shoes, commons areas, public changing areas, bathrooms, dormitory style houses, locker rooms, and public swimming pools. Athlete’s foot is difficult to treat as well because of the highly contagious and recurrent nature of the fungus.
Tinea is the same fungus that causes ringworm, and is spread by direct contact with an infected body part, contaminated clothing, or by touching other objects and body parts that have been exposed to the fungus. Because the feet are an ideal place for tinea to grow and spread, this is the most commonly affected area. It is, however, known to grow in other places. The term athlete’s foot describes tinea that grows strictly on the feet.
The most commonly infected body parts are the hands, groin, and scalp, as well as the feet. Around 70% of the population suffer from tinea infections at some point in their lives, however not all of these cases are athlete’s foot. Just like any other ailment, some people are more likely to get it than others, such as people with a history of tinea infections or other skin infections, both recurring and non-recurring ones. The extent to which a person experiences regrowth and recurrent tinea infections varies from person to person.
Sometimes people will not even know that they are infected with tinea or that they have athlete’s foot because of a lack of symptoms. However, most experience mild to moderate flaking, itching, redness, and burning. However, some of the more severe symptoms include cracking and bleeding skin, intense itching and burning, pain while walking or standing, and even blistering.
Because of the recurring nature of the tinea fungus and the athlete’s foot it causes, the best way to treat this condition is with prevention. You can take some preventative measures such as wearing flip flops or sandals in locker rooms and public showers to reduce contact with the floor. It also helps to keep clean, dry feet while allowing them to breathe. Using powders to keep your feet dry is a good idea, as well as keeping your feet exposed to light and cool air, to prevent the growth of tinea. If you do happen to get athlete’s foot, opt for using topical medicated creams, ointments or sprays. These treatments help eliminate and prevent it from coming back.
An Inflamed Nerve May Indicate Morton’s Neuroma
 The medical condition that is referred to as Morton’s neuroma generally forms in the ball of the foot, and the pain is felt between the third and fourth toes. It can develop as a result of frequently participating in high-impact sporting activities, or from wearing shoes that do not have adequate room for the toes to move freely in. This may cause the tissue surrounding the toe to thicken, which can then become inflamed and irritated. Common symptoms that patients may experience can consist of foot pain while walking, or a burning or tingling sensation. Additionally, it may feel like there is a small stone in the bottom of the foot. After a proper diagnosis is performed, which typically consists of a foot and ankle examination, correct treatment can begin. If you are affected by Morton’s neuroma, please consult with a podiatrist who can determine what the best treatment is for you.
The medical condition that is referred to as Morton’s neuroma generally forms in the ball of the foot, and the pain is felt between the third and fourth toes. It can develop as a result of frequently participating in high-impact sporting activities, or from wearing shoes that do not have adequate room for the toes to move freely in. This may cause the tissue surrounding the toe to thicken, which can then become inflamed and irritated. Common symptoms that patients may experience can consist of foot pain while walking, or a burning or tingling sensation. Additionally, it may feel like there is a small stone in the bottom of the foot. After a proper diagnosis is performed, which typically consists of a foot and ankle examination, correct treatment can begin. If you are affected by Morton’s neuroma, please consult with a podiatrist who can determine what the best treatment is for you.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Robert Marcus of Foot & Ankle Center of Teaneck. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Morton's Neuroma
A neuroma is a thickening of nerve tissue and can develop throughout the body. In the foot, the most common neuroma is a Morton’s neuroma; this typically forms between the third and fourth toes. The thickening of the nerve is typically caused by compression and irritation of the nerve; this thickening can in turn cause enlargement and, in some cases, nerve damage.
Neuromas can be caused by anything that causes compression or irritation of the nerve. A common cause is wearing shoes with tapered toe boxes or high heels that force the toes into the toe boxes. Physical activities that involve repeated pressure to the foot, such as running or basketball, can also create neuromas. Those with foot deformities, such as bunions, hammertoes, or flatfeet, are more likely to develop the condition.
Symptoms of Morton’s neuroma include tingling, burning, numbness, pain, and the feeling that either something is inside the ball of the foot or that something in one’s shoe or sock is bunched up. Symptoms typically begin gradually and can even go away temporarily by removing one’s shoes or massaging the foot. An increase in the intensity of symptoms correlates with the increasing growth of the neuroma.
Treatment for Morton’s neuroma can vary between patients and the severity of the condition. For mild to moderate cases, padding, icing, orthotics, activity modifications, shoe modifications, medications, and injection therapy may be suggested or prescribed. Patients who have not responded successfully to less invasive treatments may require surgery to properly treat their condition. The severity of your condition will determine the procedure performed and the length of recovery afterwards.
Arthritis Can Cause Pain in the Feet and Ankles
Elderly People and Falling
 Falling can be a devastating experience, and it is common among people who are aged sixty-five and older. It can cause severe foot injuries, and may compromise the quality of life. Falls can happen for a variety of reasons, including wearing shoes that do not fit correctly, muscle weakness, or safety hazards in the living environment. There are methods that can be implemented which may help to reduce the risk of falling. These can consist of having regular medical and vision examinations where existing medications can be reviewed, keeping rooms uncluttered, and installing grab bars in the shower and toilet area. If you would like more information about how falling can affect the feet, please speak to a podiatrist who can help you with proper preventive methods.
Falling can be a devastating experience, and it is common among people who are aged sixty-five and older. It can cause severe foot injuries, and may compromise the quality of life. Falls can happen for a variety of reasons, including wearing shoes that do not fit correctly, muscle weakness, or safety hazards in the living environment. There are methods that can be implemented which may help to reduce the risk of falling. These can consist of having regular medical and vision examinations where existing medications can be reviewed, keeping rooms uncluttered, and installing grab bars in the shower and toilet area. If you would like more information about how falling can affect the feet, please speak to a podiatrist who can help you with proper preventive methods.
Preventing falls among the elderly is very important. If you are older and have fallen or fear that you are prone to falling, consult with Dr. Robert Marcus from Foot & Ankle Center of Teaneck. Our doctor will assess your condition and provide you with quality advice and care.
Every 11 seconds, an elderly American is being treated in an emergency room for a fall related injury. Falls are the leading cause of head and hip injuries for those 65 and older. Due to decreases in strength, balance, senses, and lack of awareness, elderly persons are very susceptible to falling. Thankfully, there are a number of things older persons can do to prevent falls.
How to Prevent Falls
Some effective methods that older persons can do to prevent falls include:
- Enrolling in strength and balance exercise program to increase balance and strength
- Periodically having your sight and hearing checked
- Discuss any medications you have with a doctor to see if it increases the risk of falling
- Clearing the house of falling hazards and installing devices like grab bars and railings
- Utilizing a walker or cane
- Wearing shoes that provide good support and cushioning
- Talking to family members about falling and increasing awareness
Falling can be a traumatic and embarrassing experience for elderly persons; this can make them less willing to leave the house, and less willing to talk to someone about their fears of falling. Doing such things, however, will increase the likelihood of tripping or losing one’s balance. Knowing the causes of falling and how to prevent them is the best way to mitigate the risk of serious injury.
If you have any questions, please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Falls Prevention
Elderly Americans are very susceptible to falls as they get older. Everyone experiences decreases in flexibility, balance, strength, and the senses as they age. This correlates to some eye-opening statistics. 1 in 4 Americans aged 65 and older fall each year. An elderly American is being treated for a fall in an emergency room every 11 seconds. In light of these striking statistics, one can see the importance of taking steps to prevent falls.
Finding an exercise program for the elderly is an excellent way to reduce the likelihood of falls. Look for an exercise program that improves strength and balance. Elderly people who live a more sedentary lifestyle, with little physical activity, are at an increased risk of falling. Wearing well-fitted footwear that provides good foot support and cushion will help prevent falls from poorly fitted shoes. Talking to a podiatrist about your susceptibility to falls and about inspecting your prescriptions will help to avoid any medication that could make falls more likely. Due to a decline in the senses among the elderly, having your eyes and hearing checked is recommended.
Around half of all falls occur in the household. Removing tripping hazards in the home and making it more accommodating to older persons can significantly reduce falls. Some notable household changes include increasing lighting around the house, installing grab bars in the shower and bathroom, and making sure the floor is clear of clutter. Other smart options include installing a shower chair, using rubber-bottomed rugs, and placing railings on both sides of stairwells.
Finally, discuss with a doctor and your family about your fear of falling. This will help to increase awareness among the population on the need for fall prevention. A lack of awareness on the matter, and a downplaying of importance are what increase the risks of falling. Following these tips can help to reduce the risk for yourself and your loved ones.