When Walking Normally Is No Easy Feat
Walking may not seem to be a complex activity, however, several body functions, structures, and systems need to work together seamlessly to allow a person to walk normally. A person’s gait (way of walking) can be affected by genetic factors, injuries, physical abnormalities or conditions affecting the feet and legs, illnesses, inner ear problems, and age. These abnormal gait patterns may be temporary or permanent, usually falling into one of five categories. When someone drags their feet, or looks stiff while walking, this can indicate a spastic gait. When legs bend inwardly or hit each other during walking, this is known as a scissors gait. If a person’s toes scrape against or point towards the ground, they may have a steppage gait. Moving from side-to-side with short steps is indicative of a waddling gait. A propulsive gait is walking with a stooping, stiff posture, with the head and neck pushed forward. Using state-of-the-art technology, a podiatrist can perform a biomechanical assessment and gait analysis. Custom orthotics and other methods can be used to help improve feet function and ease any associated pain—including treating any underlying foot condition.
If you are having discomfort in your feet and would like to try orthotics, contact Dr. Robert Marcus from Foot & Ankle Center of Teaneck. Our doctor can provide the care you need to keep you pain-free and on your feet.
What Are Orthotics?
Orthotics are inserts you can place into your shoes to help with a variety of foot problems such as flat feet or foot pain. Orthotics provide relief and comfort for minor foot and heel pain but can’t correct serious biomechanical problems in your feet.
Over-the-Counter Inserts
Orthotics come in a wide variety of over-the-counter inserts that are used to treat foot pain, heel pain, and minor problems. For example, arch supports can be inserted into your shoes to help correct overarched or flat feet, while gel insoles are often used because they provide comfort and relief from foot and heel pain by alleviating pressure.
Prescription Orthotics
If over-the-counter inserts don’t work for you or if you have a more severe foot concern, it is possible to have your podiatrist prescribe custom orthotics. These high-quality inserts are designed to treat problems such as abnormal motion, plantar fasciitis, and severe forms of heel pain. They can even be used to help patients suffering from diabetes by treating foot ulcers and painful calluses and are usually molded to your feet individually, which allows them to provide full support and comfort.
If you are experiencing minor to severe foot or heel pain, it’s recommended to speak with your podiatrist about the possibilities of using orthotics. A podiatrist can determine which type of orthotic is right for you and allow you to take the first steps towards being pain-free.
If you have any questions please contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ankle Foot Orthotics for Athletes
Ankle foot orthotics are shoe inserts that offer support to control the placement and movement of the ankle, correct deformities, and compensate for weakness. These inserts are used to stabilize the foot and ankle and provide toe clearance during the swing phase of gate.
Athletes often suffer foot problems because their feet are not being supported within the shoe. Ankle and foot orthotics are custom made inserts that alleviate stress on the foot. However custom orthotics should be prescribed by a podiatrist who specializes in customized footwear and orthotics design. These inserts are used by athletes for different reasons. Runners use orthotics to absorb shock at heel contact and to set up the forefoot for push-off. Basketball players wear them to control their forefeet while jumping and running.
The two main types of orthotics are over-the-counter orthotics and custom-made orthotics. To be eligible for custom orthotics, an examination of the foot and ankle will need to be completed. Afterward, both the foot and ankle will need to be casted and fitted for the proper orthotic. When the fitting process is complete, adjustments can be made to make sure everything fits perfectly.
Over the counter orthotics tend to be more popular than custom fit ones. Athletes who have less severe aches and pains in the foot, ankle or lower back area can use the over-the-counter version of orthotics. Unfortunately, over-the-counter orthotics tend to not work in treating severe injuries or ailments. Whenever you suspect you may need an ankle foot orthotic, you should consult with your podiatrist to determine which type of orthotic is right for you.
Types of Foot Blisters
Blisters are fluid-filled bubbles of skin that can form anywhere on the body. Most blisters on the feet and toes are caused by friction from shoes or socks rubbing repeatedly over a concentrated area of skin. The top layer of skin separates from the layers of skin underneath it and the empty space fills with a fluid called serum or plasma. The fluid cushions and protects the raw skin underneath the blister. Most blisters are clear and filled with serum. Sometimes, a blister can appear red or black. This is indicative of blood vessel damage, in addition to skin damage. Infected blisters may have a white or yellow tinge due to pus forming and collecting beneath the blister. Most blisters heal on their own, but if you have a blister that appears to be infected, it is strongly suggested that you see a podiatrist for treatment.
Blisters are prone to making everyday activities extremely uncomfortable. If your feet are hurting, contact Dr. Robert Marcus of Foot & Ankle Center of Teaneck. Our doctor can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters develop as a result of constantly wearing tight or ill-fitting footwear. This happens due to the constant rubbing from the shoe, which can often lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
How Do Blisters Form?
Blisters on the feet are often the result of constant friction of skin and material, usually by shoe rubbing. Walking in sandals, boots, or shoes that don’t fit properly for long periods of time can result in a blister. Having consistent foot moisture and humidity can easily lead to blister formation.
Prevention & Treatment
It is important to properly care for the affected area in order to prevent infection and ease the pain. Do not lance the blister and use a Band-Aid to provide pain relief. Also, be sure to keep your feet dry and wear proper fitting shoes. If you see blood or pus in a blister, seek assistance from a podiatrist.
If you have any questions, please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are small pockets of fluid that occur on the top layers of the skin for several reasons. Friction, burns, and diseases are all known causes of blisters. Smaller blisters are known as vesicles, while larger blisters are referred to as bulla. The fluid inside the bubble can be blood, pus, or serum; which is a clear liquid that protects the skin. In most cases, blisters are not a major health issue, but they can be an indicator of a more serious condition.
Causes of blisters vary. Blisters are commonly caused by wearing poorly fitted shoes that rub against the foot. However, there are many other causes besides from friction; including burns, sunburn, insect bites, frostbite, poison ivy/oak, chemical exposure, impetigo, eczema, viral infections, and more.
Most blisters heal by themselves and do not require immediate medical care. If you have a blister, do not pop it since this may cause infection; it is advised to put a bandage over the blister to protect it. If the blister is large, causes pain, or if you have a fever, it is recommended that you see a doctor who can provide proper care. Blisters are easy to diagnose, and if considered prudent by the doctor, can easily be drained of fluid with a sterile needle as well.
To prevent blisters on the feet, wear shoes that fit properly and don’t cause rubbing. Socks can help prevent friction and it is recommended that you wear them if you are wearing shoes. Hand blisters can be avoided by wearing gloves during activities that cause friction against the hand. If you have a blister that pops, do not remove the dead skin, wash the area, apply antibiotic ointment, and cover with a bandage. It is okay in most cases to not seek immediate medical care for a blister if it was just caused by friction. However, if the blister causes pain or does not go away, it is suggested that you see a doctor for a diagnosis.
Is My Ingrown Toenail Infected?
 Ingrown toenails occur when a toenail grows into the surrounding skin instead of over it. While many cases of ingrown toenails can be resolved without complications, it is important to stay on the lookout for any signs of infection. These may include reddening or hardening of the skin surrounding the ingrown nail, swelling, pain, pressure under the nail, throbbing, bleeding, a foul odor, a buildup of fluid, and warmth around the nail. In more severe infections, pus-filled abscesses can form where the nail pokes into the skin. If your ingrown toenail is showing signs of infection, it is suggested that you see a podiatrist as soon as possible.
Ingrown toenails occur when a toenail grows into the surrounding skin instead of over it. While many cases of ingrown toenails can be resolved without complications, it is important to stay on the lookout for any signs of infection. These may include reddening or hardening of the skin surrounding the ingrown nail, swelling, pain, pressure under the nail, throbbing, bleeding, a foul odor, a buildup of fluid, and warmth around the nail. In more severe infections, pus-filled abscesses can form where the nail pokes into the skin. If your ingrown toenail is showing signs of infection, it is suggested that you see a podiatrist as soon as possible.
Ingrown toenails can become painful if they are not treated properly. For more information about ingrown toenails, contact Dr. Robert Marcus of Foot & Ankle Center of Teaneck. Our doctor can provide the care you need to keep you pain-free and on your feet.
Ingrown Toenails
Ingrown toenails occur when a toenail grows sideways into the bed of the nail, causing pain, swelling, and possibly infection.
Causes
- Bacterial infections
- Improper nail cutting such as cutting it too short or not straight across
- Trauma to the toe, such as stubbing, which causes the nail to grow back irregularly
- Ill-fitting shoes that bunch the toes too close together
- Genetic predisposition
Prevention
Because ingrown toenails are not something found outside of shoe-wearing cultures, going barefoot as often as possible will decrease the likeliness of developing ingrown toenails. Wearing proper fitting shoes and using proper cutting techniques will also help decrease your risk of developing ingrown toenails.
Treatment
Ingrown toenails are a very treatable foot condition. In minor cases, soaking the affected area in salt or antibacterial soaps will not only help with the ingrown nail itself, but also help prevent any infections from occurring. In more severe cases, surgery is an option. In either case, speaking to your podiatrist about this condition will help you get a better understanding of specific treatment options that are right for you.
If you have any questions please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Ingrown Toenails
An ingrown toenail is a nail that has curved downward and grown into the skin. This typically occurs at either the nail borders or the sides of the nail. As a result, pain, redness, swelling, and warmth may occur in the toe. If a break in the skin forms due to the ingrown nail, bacteria may enter and cause an infection in the area; this is typically characterized by a foul odor and drainage.
Ingrown toenails have multiple reasons for developing. In many instances, the condition is a result of genetics and is inherited. The most common cause, however, is improper trimming; cutting the toenails too short forces the skin beside the nail to fold over. An ingrown toenail can also develop due to trauma, such as stubbing the toe, having an object fall on the toe, or participating in activities that involve repeated kicking or running. Wearing shoes that are too tight or too short can also cause ingrown toenails.
Treatment for an ingrown toenail varies between patients and the severity of the condition. In most cases, it is best to see your podiatrist for thorough and proper treatment. After examining your toe, your podiatrist may prescribe oral antibiotics to clear the infection if one is present. Surgical removal of either a portion of the nail or the entire nail may also be considered. In some cases, complete removal or destruction of the nail root may be required. Most patients who undergo nail surgery experience minimal pain afterward and can return to normal activity the following day.
Ingrown toenails can be prevented with proper nail trimming and by avoiding improper-fitting shoes. When cutting the toenails, be sure that you are cutting in a straight line and avoid cutting them too short. Shoes should not be too short or tight in the toe box.
Why Live with Pain and Numbness in Your Feet?
Common Causes of Heel Pain in Children
 Children are often on their feet playing games, participating in sports, and running and jumping around. High levels of activity can increase your child’s chances of developing heel pain. Active children between the ages of 8 and 14 may find themselves with Sever’s disease, an inflammation of the growth plate in the heel. Plantar fasciitis, an inflammation of the ligament that runs along the bottom of the foot, is also common. Children who play high impact sports like football may be more likely to incur Achilles tendon injuries or foot and ankle fractures. If your child complains of heel pain, take them to see a podiatrist. With proper care, your child can make a full recovery.
Children are often on their feet playing games, participating in sports, and running and jumping around. High levels of activity can increase your child’s chances of developing heel pain. Active children between the ages of 8 and 14 may find themselves with Sever’s disease, an inflammation of the growth plate in the heel. Plantar fasciitis, an inflammation of the ligament that runs along the bottom of the foot, is also common. Children who play high impact sports like football may be more likely to incur Achilles tendon injuries or foot and ankle fractures. If your child complains of heel pain, take them to see a podiatrist. With proper care, your child can make a full recovery.
Many people suffer from bouts of heel pain. For more information, contact Dr. Robert Marcus of Foot & Ankle Center of Teaneck. Our doctor can provide the care you need to keep you pain-free and on your feet.
Causes of Heel Pain
Heel pain is often associated with plantar fasciitis. The plantar fascia is a band of tissues that extends along the bottom of the foot. A rip or tear in this ligament can cause inflammation of the tissue.
Achilles tendonitis is another cause of heel pain. Inflammation of the Achilles tendon will cause pain from fractures and muscle tearing. Lack of flexibility is also another symptom.
Heel spurs are another cause of pain. When the tissues of the plantar fascia undergo a great deal of stress, it can lead to ligament separation from the heel bone, causing heel spurs.
Why Might Heel Pain Occur?
- Wearing ill-fitting shoes
- Wearing non-supportive shoes
- Weight change
- Excessive running
Treatments
Heel pain should be treated as soon as possible for immediate results. Keeping your feet in a stress-free environment will help. If you suffer from Achilles tendonitis or plantar fasciitis, applying ice will reduce the swelling. Stretching before an exercise like running will help the muscles. Using all these tips will help make heel pain a condition of the past.
If you have any questions please contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Heel Pain
Heel pain can be difficult to deal with, especially if you do not know what the underlying cause is. If you ignore your heel pain, the pain can magnify and potentially develop into a chronic condition. Depending on the location of your heel pain, you have developed a specific condition.
One condition is plantar fasciitis. Plantar fasciitis is caused by the inflammation of the plantar fascia, or the band of tissue that connects the heel bone to the base of the toes. The pain from this condition is initially mild but can intensify as more steps are taken when you wake up in the morning. To treat this condition, medication will likely be necessary. Plantar fasciitis is often associated with heel spurs; both require rest and special stretching exercises.
There are various options your podiatrist may suggest for heel pain. Treatment options for heel pain typically include non-steroidal anti-inflammatory drugs (NSAIDS), which may reduce swelling and pain. Other options are physical therapy, athletic taping, and orthotics. In severe cases of heel pain, surgery may be required.
Preventing heel pain is possible. If you are looking to prevent heel pain from developing in the future, be sure to wear shoes that fit you properly and do not have worn down heels or soles. Be sure to warm up properly before participating in strenuous activities or sports that place a lot of a stress on the heels. If you are experiencing any form of heel pain, speak with your podiatrist to determine the underlying cause and receive the treatment you need.
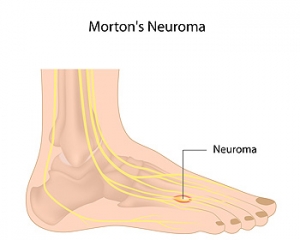
Morton’s Neuroma Causes Burning Pain
Morton’s neuroma refers to the thickening or scarring of a nerve in the ball of the foot. This condition typically affects the nerve located between the third and fourth toes. When the nerve is compressed or irritated, the nerve tissue can thicken and scar, causing a variety of painful symptoms. If left untreated, nerve damage may become permanent. Symptoms of Morton’s neuroma include burning pain in the ball of the foot, tingling, numbness, and the feeling of walking on a pebble. Symptoms usually worsen while walking, bearing weight on the affected foot, or wearing tight shoes. If you are experiencing the symptoms of Morton’s neuroma, please seek the care of a podiatrist.
Morton’s neuroma is a very uncomfortable condition to live with. If you think you have Morton’s neuroma, contact Dr. Robert Marcus of Foot & Ankle Center of Teaneck. Our doctor will attend to all of your foot care needs and answer any of your related questions.
Morton’s Neuroma
Morton's neuroma is a painful foot condition that commonly affects the areas between the second and third or third and fourth toe, although other areas of the foot are also susceptible. Morton’s neuroma is caused by an inflamed nerve in the foot that is being squeezed and aggravated by surrounding bones.
What Increases the Chances of Having Morton’s Neuroma?
- Ill-fitting high heels or shoes that add pressure to the toe or foot
- Jogging, running or any sport that involves constant impact to the foot
- Flat feet, bunions, and any other foot deformities
Morton’s neuroma is a very treatable condition. Orthotics and shoe inserts can often be used to alleviate the pain on the forefront of the feet. In more severe cases, corticosteroids can also be prescribed. In order to figure out the best treatment for your neuroma, it’s recommended to seek the care of a podiatrist who can diagnose your condition and provide different treatment options.
If you have any questions, please feel free to contact our office located in Teaneck, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.